SKYGEN

AUTHORS: Marcel Tetzlaff, SKYGEN’s VP of Provider Experience and Dental Benefits Management and Judy Greenlea Taylor, DDS, MPH, FICD, FACD, Dental Director, CareSource Georgia
Robust analytics and innovative value-based dental plan models can help payers optimize dental plan performance, improve care, optimize benefit costs, and boost provider engagement.
SKYGEN recently partnered with the National Association of Dental Plans (NADP) to share strategies for using analytics and implementing value-based dental programs to improve dental plan performance.
In the webinar we discussed how to:
- Improve the efficiency and appropriateness of care by identifying and encouraging best practices and creating provider education opportunities to minimize fraud, waste and abuse (FWA) and inappropriate care
- Give members access to quality care by identifying and rewarding high-performing providers
- Discover opportunities for optimizing benefit costs through reimbursement analysis
- Elevate the provider experience by rewarding dentists who meet higher standards and designing creative benefit plans
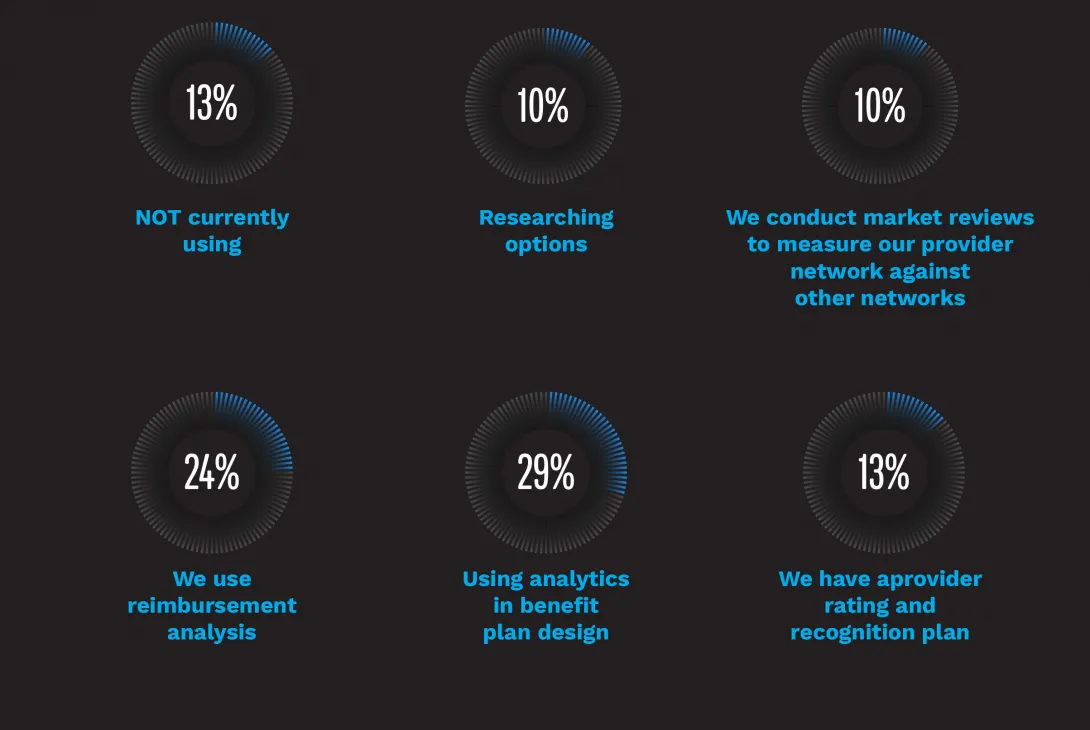
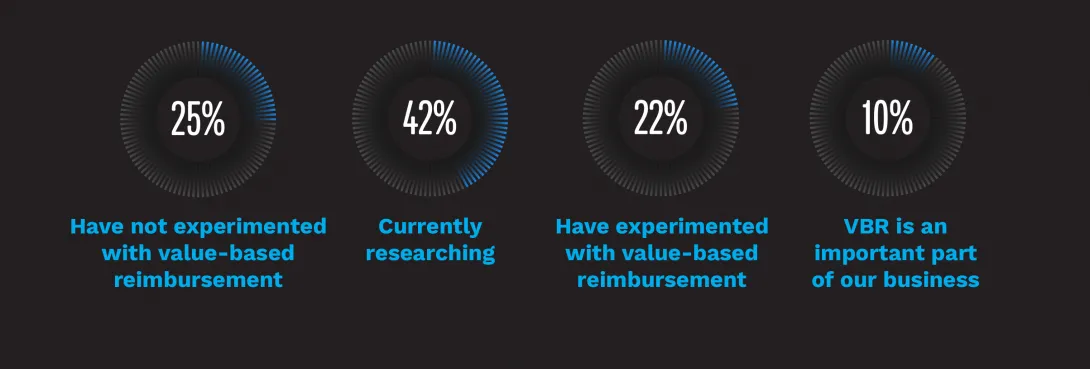
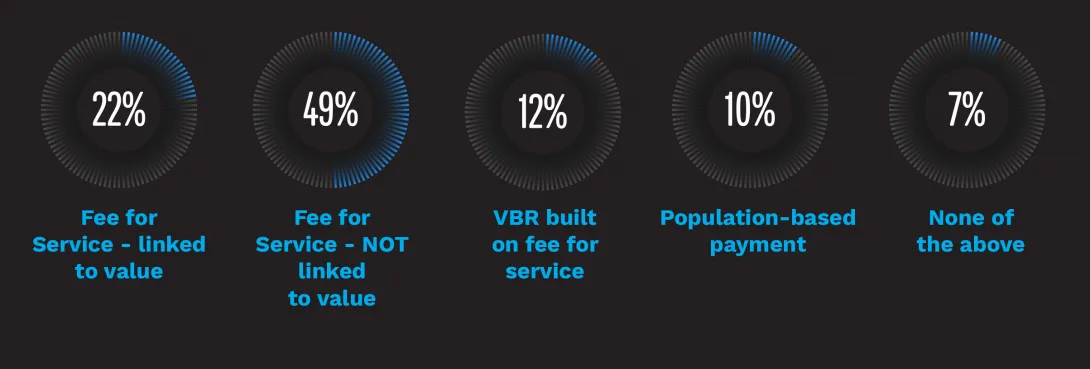
Surveys of webinar attendees show that most are using analytics to improve the performance of their dental plans. In addition, while value-based reimbursement is still not widely used among attendees, many are researching their options. Of those who are using value-based reimbursement some type of fee for service (FFS) program is most common.
POLL QUESTIONS ANSWERED DURING THE WEBINAR...
poll: Are you using analytics to improve the performance of your Dental Plans?
poll: Have you experimented with value-based reimbursement?
poll: We currently employ the following types of value-based reimbursement.
Q&A WITH THE SPEAKERS
The webinar generated tremendous interest and we wanted to take this opportunity to address questions that were raised during the presentation.
Q: How do Medicaid plans get on board with value-based reimbursement especially if there is a dental vendor involved?
The health plan may develop the VBR program and allow the dental vendor to implement, or the vendor may develop and implement a VBR for the health plan based on the goals, funding and shared overall strategy. A VBR project plan would include calculations and measurement of providers as well as provider communication.
Q: How long should a small-scale test last and what factors should we consider when selecting a time frame?
Most programs are built on quarterly payments to providers, so after each three-month period, the test program could be evaluated and changes made as appropriate. However, if a primary metric goal for evaluation and calculation of payment is to promote preventive services, due to the nature of preventive dentistry (i.e. recall and cleanings every six months) some data may not be captured in less than a six-month period. In addition, a sample test can be done using data from the previous year which can help identify the right measurements, the cost/savings and testing of the overall analysis and payment.
Q: How are customers (member groups) responding to value-based?
There is a great deal of discussion and research in the dental industry around value-based programs. Value-based payment models have expanded extensively and become the predominant payment model over FFS for most Medicaid medical arenas with the advent of HEDIS® requirements. It is growing in both behavioral health and oral health services. Appropriate program design, measurements and cost analytics can help ensure that a VBR program will reduce overall costs and improve outcomes.
Q: What recommendations do you have to get providers engaged when implementing a value-based program?
Providers understand VBR at a high level and know that it will eventually become the norm. Transparency in the analytics, methodology and provider performance data will help providers feel engaged as well as give them a roadmap for success in a VBR model. It is recommended that you involve a small focus group of providers to help design and implement a VBR program.
Q: What provider education programs are the most effective in combatting FWA?
Provider education is key and can consist of anything from provider newsletter articles to webinars to in-person, one-on-one meetings. Providing transparency that outliers and abnormal patterns are based on peer-to-peer, geographic and other normalizing comparisons helps providers understand better. The specific issues identified through FWA analysis will determine the best method of intervention. We recommend an escalating approach. If potential issues are found early, a simple conversation between the provider relations rep and provider would be the first step. If not resolved or if it progresses, next steps would include a peer-to-peer conversation, written notification and eventually a formal chart audit. An approach may even include helping providers self-evaluate by setting up in-office compliance programs and a practice compliance officer to understand and maintain policy guidelines.
Q: What are the most effective tools for provider recognition programs?
Provider recognition can be separated into financial and non-financial. Financial recognition via an incentive payment is usually the most effective. Non-financial recognition that is most effective enlists a rating system which allows providers to indicate they are a preferred or high performing provider, and steering members to those providers via the contact center or web site. This scenario benefits all stakeholders – member, provider and payer. Another non-financial incentive might include waiving certain administrative processes (i.e. prior authorization of certain procedures).
Q: Who supplies the data for use in VBR programs and how much baseline data do you need for valid analysis?
Primarily the data comes dental claims, authorization or complaints from the health plan or dental vendor. We recommend including at least one year of statistically valid data.
If data other than dental-specific data is available and can be incorporated into the calculation, that would be ideal. In most cases there isn’t true integration between medical, pharmacy and other health services. Sometimes ICD 10 diagnosis codes can be used to identify health status comparisons, high risks, etc. but this is beneficial when it can be gleaned across all claims. Only a few states require usage for dental claims. However, even with just dental data, there is an opportunity to make adjustments due to a member’s oral health status if you can include caries risk assessments, special needs or other factors.
Q: What methods do you use to deal with regional or market specific characteristics?
Most often, a provider is compared to his/her peer group, at a regional, state or national level, based on specialty or types of services rendered. In addition, individual characteristics should be taken into consideration.
Q: Why should we consider outsourcing analysis of our plan performance?
Outsourcing to an experienced vendor can assist with comparison to national or other benchmarks, improve the amount and quality comparison data as well as lend overall clinical and data analytics expertise.
Interested in learning more?
Watch the full webinar now.
Latest Blog Posts
Learn how you can transform the delivery of health benefits with SKYGEN.